Things You Can Do as a Long-Distance Caregiver
If you live far away from a family member or friend who needs care, here are some tips on things you can do.
Ecumen Bethany Community’s Lori Zastrow: Caregiver of the Year
 Lori Zastrow of Ecumen Bethany Community was named a LeadingAge Minnesota Caregiver of the Year.
Lori Zastrow of Ecumen Bethany Community was named a LeadingAge Minnesota Caregiver of the Year.
Honoring Ecumen’s Longest Tenured Employee: Dawn Bolhuis, LPN, Kindhearted and Compassionate Nurse
 Nurse Dawn Bolhuis, Ecumen's longest tenured employee, can't wait to start her next shift, and the residents she cares for can't wait to see her.
Nurse Dawn Bolhuis, Ecumen's longest tenured employee, can't wait to start her next shift, and the residents she cares for can't wait to see her.
Thankful Family Honors Grand Village Caregivers
Her phone was ringing off the hook. Roberta Alzen, the director of nursing at Ecumen-managed Grand Village in Grand Rapids, Minn., was caught off guard.
“Have you seen the paper?” the callers all wanted to know. She had not, but would quickly find out that she and the staff at Grand Village were being honored in a deeply touching way.
Prominently displayed on the editorial page of the Sunday Grand Rapids Herald Review was a letter from a grieving mother who had just lost her son.
Dottie Wilde of Grand Rapids had just said goodbye to her son, Donald. He was only 55. In 2012 he had a stroke and never fully recovered.
Now she wanted everyone in the community to know how well he had been cared for the last two years of his life at Grand Village — two very difficult years. “I was so thankful he was in such a good home and he got the best care he could have received,” Dottie wrote. “Everyone is so caring and so kind and they give such good nursing care to everyone.”
What made this appreciation so much more meaningful was Dottie’s background. “I spent 42 years in nursing myself,” she wrote, “so I feel I know what good patient care is. I feel the nursing staff not only takes care of the residents and patients but they also take care of the families of the residents.”
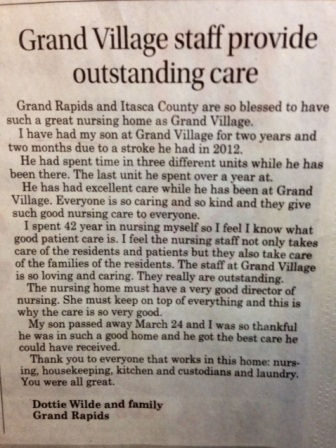 And there was special mention of Roberta, as the director of nursing. “She must keep on top of everything and this is why the care is so very good,” Dottie wrote. And she concluded: “Thank you to everyone that works in this home: nursing, housekeeping, kitchen and custodians and laundry. You were all great.”
And there was special mention of Roberta, as the director of nursing. “She must keep on top of everything and this is why the care is so very good,” Dottie wrote. And she concluded: “Thank you to everyone that works in this home: nursing, housekeeping, kitchen and custodians and laundry. You were all great.”
Roberta said everyone at Grand Village was moved by such heartfelt and public thanks. She said because Donnie was so young and had so many challenges, he was a special member of the community. Everyone got involved in his care, and he, in turn, did what he could to help take care of the older members of the community.
“We all worked as a team,” Roberta said.
In this small community, Roberta said sometimes family members of residents will recognize her on the street and give her a hug. But this is the first time she and her staff have been honored so publicly.
And it means a lot. She said everyone on the staff learned from the journey with Donnie. And then — that day when they picked up the paper — they learned just how much what they did really mattered.
How To Be a Good Caregiver When the Caregivee Doesn’t Want Your Help
How can you be a good caregiver to someone who is not happy to have your help? The “reluctant caregivee” is a common challenge to caregivers, even those who are close family members. Few people like the idea of relying on another person for basic needs and tend to resist even when they desperately need help.
Here’s some detailed advice from Caring.com on how to graciously give care when your help is not appreciated.
A Caregiver Support Group Innovation Hits Its Stride
Sometimes a good talk with someone who understands helps relieve the stress of caregiving. In fact, that is the basis of most support groups.
Just pulling the chairs in a circle and sharing frustrations seems to work for many people. Now a California caregiver support group has taken this simple approach to the next level by adding on another simple idea. “Meet and Move” is a support group on the go — walking, talking and sharing.
Rather than sitting, the group hikes in scenic areas, and the exercise offers an added dimension of stress relief.
The New York Times New Old Age Blog tells the story of “Meet and Move” and its enthusiastic participants, who say they are becoming better caregivers by also taking care of themselves.
A Must-Read: Washington Post Brings Caregiving Crisis Front and Center
If you’re not already a caregiver to a loved one, chances are high you will be one day. The constellation of issues you are, or will be, facing are daunting. And even if you’re never in this role, the looming crisis is sure to have major societal effects that will impact everyone.
The Washington Post recently took an in-depth look at caregiving and published “Caregiving: A Special Report” highlighting the current and future issues Americans face as more people live longer and there are fewer younger people and fewer financial resources to take care of them. The Post held “Caregiving in America” forums in Chicago and Seattle and interviewed experts in all aspects of the caregiving crisis.
As former First Lady Rosalynn Carter puts it: "There are only four kinds of people in the world: those who have been caregivers, those who are currently caregivers, those who will be caregivers, and those who will need caregivers."
Travel writer and TV host Rick Steves in a video interview offers a heartfelt plea for action: “As our society becomes more successful… living longer and out-living our brains or bodies… loved ones are taking care of loved ones… It’s a big issue that people don’t talk about so much… but there’s so much power and passion and affluence in our society. If we can’t deal with this in a smart and honest way, it’s sort of an embarrassment for our whole society. The caliber of a great nation is how they deal with seniors…”
The Post’s report is comprehensive — full of information that honors and empowers caregivers and takes on the rapidly emerging personal and societal issues. Both printed and online versions are available at the links below:
An Ecumen Consultant’s Quest To Make Sense of Dementia
Tom Stober, an expert on process and efficiency, was routinely going about his work one day when he walked into a room and came face-to-face with something that “shook me to the core.” It was not logical. It was not rational. The normal rules of organization did not apply. On some deep level, it rocked his orderly world.
It was a memory care community, where residents with dementia live.
Tom works for Minnesota Lean Partners, which had been hired by Ecumen over a year ago to improve customer experiences by teaching staff how to focus on what is truly important—what really adds value— and eliminating unnecessary things that get in the way of that goal. This was his first consulting assignment in senior services. A mechanical engineer by training, Tom had worked for many manufacturing companies, most notably Toyota, where he first learned the principles of “lean” management from the masters.
The Ecumen training sessions Tom was conducting were going well. He was teaching, and he was learning. But that first exposure to memory care was life-changing for him.
“I had heard about Alzheimer’s and dementia,” he says, “but I was never truly exposed to the impact that this has on the residents as well as their families.”
After visiting the memory care community at Ecumen Detroit Lakes, Tom remembers going to his hotel room that night preoccupied with his experience. He just could not get it out of his mind. “I was troubled by the degree that this bothered me. I struggled with the fact that these crippling diseases destroy what was once functioning human beings as mothers, fathers, sisters and brothers.”
There was just no apparent logic to it.
Yet as Tom watched the caregivers at work, he was in awe of “how loving, caring and forgiving” they were— and how effective.
“I was amazed at the strength and caring of the Ecumen staff working in this environment day-in and day-out,” Tom recalls. “Being briefly exposed to some of the behaviors that Ecumen care providers experience daily, it had a sincere and profound impact on me. I have a much higher appreciation for their contributions to the organization and their dedication to providing a high quality care to those that truly need it.”
A powerful emotion swept over him. “What I saw made me more dedicated to the work Ecumen is doing and made me want to help the staff more,” he recalls.
“I know caregiving is a job I could not do,” Tom says. “It takes a certain type of person.”
But he realized he is the certain type of person who could make caregivers’ jobs easier. That could be his way of coming to terms and making a contribution.
From Tom’s point of view, you can always make things better with organization, standardization and elimination of useless and wasteful practices—whether in a manufacturing plant or a memory care community.
“This could be my small way of paying it forward,” he decided.
On the most basic level, he noticed right away that caregivers spent a lot of time just looking for things they needed, often going in and out of rooms several times looking for supplies and equipment. So he helped staff systematically figure out how to put all the tools of care in the same place in every room. With everything they need easy to find, they are freed up to spend more time in direct care.
Then he started digging deeper. How can we organize care around the biorhythms of the residents? When is the best time of day to have activities? How can space best be used to optimize residents’ enjoyment? How can we improve the residents’ environment and create better experiences? Recently, he worked with the memory care staff at Ecumen Pathstone Living in Mankato, Minn., to completely revamp the memory care community. Go to Ecumen’s Changing Aging blog to read about this effort.
Over the past year and a half, Tom has trained more than 1,000 Ecumen employees in “lean” principles and has run more than 40 events to analyze situations and implement continuous improvements. And his work continues— not only in creating better practices but also sustaining them.
As Tom was working with Ecumen and coming to grips with his reaction to observing dementia firsthand, his personal story took another turn. Tom learned that his own father is now in the early stages of dementia.
The lean management expert bonded with the dementia experts at Ecumen.
“I have gained so much knowledge about dementia,” Tom says. “The Ecumen nurses have really helped me better understand what is happening with my father, and how it’s happening and the progression to expect moving forward.”
And the paying it forward continues.
—
Ecumen received a Performance-based Incentive Payment Program (PIPP) award from the Minnesota Department of Human Services beginning October 1, 2011 - September 30, 2015. LEAN the Ecumen Way is a company-wide initiative to improve the way Ecumen delivers services in day-to-day operations. LEAN focuses on eliminating non-value added activities in our work— “wastes,” which get in the way of the more important value-added activities that customers desire.
In addition to improving resident experiences by introducing LEAN management techniques, Ecumen has pledged to reduce antipsychotics among people with dementia and improve lives in all Ecumen nursing homes through its Awakenings program (see Ecumenawakenings.org). In 2010, Ecumen was awarded a three-year performance-based grant from the State of Minnesota’s Department of Human Services to expand its pilot Awakenings program to Ecumen’s 15 nursing homes. Such grants help organizations expand innovative, results-based initiatives. These homes serve more than 1,000 people, including some of society’s most challenging dementia cases. The Minneapolis Star Tribune recently profiled the Awakenings program.








